A woman and doctor discussing early puberty and childbirth health risks
New studies link early puberty and childbirth or teen childbirth to higher long-term health risks in women. Learn the evidence, reasons, and steps to reduce risk.
Study Reveals Early Puberty and Childbirth May Cause Several Health Risks in Women
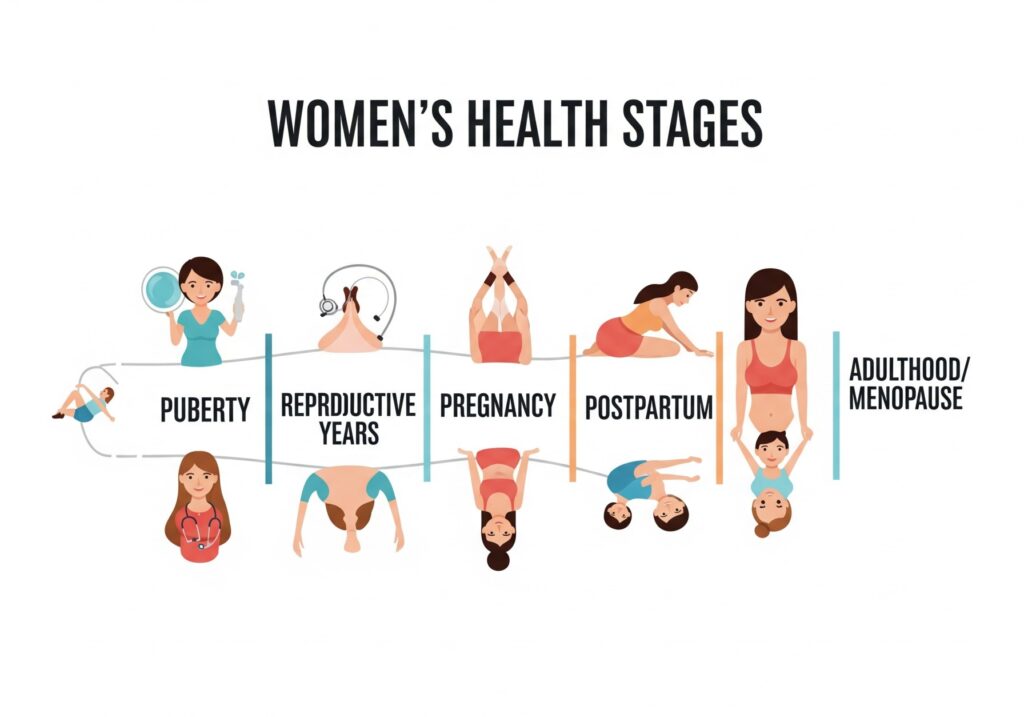
Women’s health is shaped by critical milestones. Two of the most important are the timing of first period and age at first birth. New research suggests that when these happen very early, risks rise. But there is good news. With the right care, many risks can be lowered. Here’s what the latest science says—and what you can do about it.
Why timing matters
Puberty flips powerful hormonal switches. So does pregnancy. When either occurs unusually early, the body may face extra strain. Several large studies now connect early puberty and teenage childbirth with higher chances of later health problems, including heart and metabolic disease. At the same time, researchers stress nuance: not every study agrees, and social factors matter. Understanding the evidence helps you make informed choices and seek timely care. PBS, Nature, Oxford Academic
What the research shows about early puberty and childbirth health risks
Early puberty: long-term patterns to watch
Multiple reviews and meta-analyses link the age at menarche (first period) to future cardiovascular risk. Some show a J-shaped pattern: both very early and very late menarche are associated with higher cardiovascular events. Others specifically flag early menarche as a risk marker even after considering body mass index and age. More recently, a large individual-level meta-analysis confirmed that both early and late menarche carry higher cardiovascular risk compared with mid-range timing. Frontiers, Nature, Oxford Academic
In 2025, researchers presented new data at the Endocrine Society’s annual meeting. Women who had their first period before age 10 were more likely to develop obesity, high blood pressure, diabetes, and some pregnancy complications later in life. Media coverage has highlighted these findings as part of a broader trend toward earlier puberty. Endocrine Society, PBS
That said, science evolves. One 2024 meta-analysis reported that early menarche might be protective against major adverse cardiovascular events, underscoring how results can differ by population and method. The overall takeaway is careful: timing of menarche is a risk marker, not a diagnosis, and it should be interpreted alongside other factors such as weight, blood pressure, lipids, and family history. PMC
Early childbirth: risks for mother and child
Teen pregnancy carries higher medical risks for mothers and babies. The World Health Organization reports that girls aged 10–19 face increased risks of eclampsia, infection, and other complications. Their babies face higher risks of low birth weight and preterm birth. UNICEF’s 2024 data brief adds global context: about 13% of adolescent girls and young women give birth before age 18, with far higher rates in parts of sub-Saharan Africa. World Health Organization, UNICEF DATA
Importantly, risks can echo into adulthood. A 2024 study in JAMA Network Open linked teen pregnancy with a higher risk of premature mortality in early adulthood. Other research connects pregnancy complications such as preterm birth with future cardiovascular mortality in mothers—even when births occur at “early term.” JAMA Network, AHA Journals, PubMed
How early puberty might raise risk
Why would early puberty matter so much? Scientists point to longer lifetime exposure to sex hormones, which may influence body fat, blood pressure, and cholesterol. Earlier puberty also tends to track with childhood obesity, stress, and environmental exposures, which themselves affect health. Journalistic summaries and expert panels have emphasized likely contributions from obesity and endocrine-disrupting chemicals, though causation is still being untangled. News-Medical Vox
How early childbirth may affect long-term health
Teen pregnancies are more likely to be unplanned and to occur in settings with fewer resources. As a result, prenatal care may be delayed. This can raise risks of hypertensive disorders, anemia, and postpartum depression. Several reviews document higher rates of adverse outcomes for adolescent mothers and their babies. Over the long term, pregnancy complications—especially preterm birth—are associated with increased maternal cardiovascular risk. PMC+1, AHA Journals
Practical steps to lower early puberty and childbirth health risks

For girls with early puberty (and their families)
- Seek medical guidance early. If puberty starts before age 8–9, talk to a pediatrician or pediatric endocrinologist. They can evaluate growth, hormones, and potential underlying conditions. Media coverage notes earlier puberty trends; clinicians can separate concern from urgency. PBS
- Address modifiable risks. Support healthy sleep, nutrition, and physical activity. These help with weight, blood pressure, and lipid control—factors that track into adulthood. News-Medical
- Limit harmful exposures. Experts advise practical steps to reduce endocrine-disrupting chemical exposure (e.g., avoid unnecessary fragranced products, follow food safety guidance), while warning against extreme, restrictive diets. Vox
- Plan ongoing prevention. As teens age, routine checks for BMI, blood pressure, and lipids help offset later cardiovascular risk associated with very early or very late menarche. Recent analyses support a life-course prevention mindset. Nature, Oxford Academic
For adolescents at risk of early pregnancy
- Prioritize comprehensive sex education and contraception access. The CDC notes historic declines in U.S. teen birth rates, partly due to better contraception. Professional groups like ACOG provide guidance on counseling adolescents and expanding access to reliable methods. CDC, ACOG
- Engage in early, tailored prenatal care if pregnant. Early visits catch hypertension, infections, and nutritional issues sooner. New guidance is pushing toward more personalized prenatal care models. ACOG
- Monitor for hypertensive disorders and preterm birth risks. These complications are tied to later cardiovascular disease. Post-pregnancy follow-up should include blood pressure and metabolic screening. AHA Journals
- Support education and social services. UNICEF stresses that early childbearing can derail schooling and livelihoods, compounding health risks. Linking teens to social supports can improve outcomes for mother and child. UNICEF DATA
What to ask your clinician
- “My first period was very early/late. How should that inform my heart-health screening plan?” Recent science supports discussing blood pressure, cholesterol, diabetes screening, and healthy weight goals. Nature, Oxford Academic
- “I had a preterm birth as a teen. What does that mean for my long-term heart risk?” Evidence ties preterm delivery—even early-term births—to higher cardiovascular mortality; clinicians can personalize prevention. PubMed
- “What contraception is safest and most effective for me?” ACOG maintains up-to-date clinical guidance on options for adolescents and young adults. ACOG
The bottom line on early puberty and childbirth health risks
Early puberty and adolescent childbirth do not doom anyone to poor health. But they are important signals. The strongest evidence links them—directly or through complications like preterm birth—to higher cardiometabolic risk later on. Therefore, prevention and follow-up matter. With timely counseling, equitable access to contraception, early prenatal care, and long-term heart-health screening, many risks can be reduced.
Sources and further reading (open access or summaries where possible)
- Frontiers in Pediatrics review on early puberty and cardiovascular risk. Frontiers
- Nature Scientific Reports meta-analysis: J-shaped association between age at menarche and cardiovascular events. Nature
- Press release (Endocrine Society 2025): early and late menarche linked to later health risks; media overview. Endocrine Society, PBS
- JAMA Network Open (2024): Teen pregnancy and premature mortality. JAMA Network
- American Heart Association scientific statement on adverse pregnancy outcomes and later cardiovascular disease. AHA Journals
- WHO fact sheet on adolescent pregnancy. World Health Organization
- UNICEF data brief on early childbearing. UNICEF DATA
- Research linking preterm birth and later maternal cardiovascular mortality, including early-term births. PubMed
- Reviews on adolescent pregnancy outcomes and risks. PMC+1
Helpful external links:
- WHO: Adolescent pregnancy facts and resources. World Health Organization
- CDC: Teen pregnancy overview and statistics. CDC
- ACOG: Adolescent health and contraception counseling. ACOG
Medical Disclaimer: This article is for general information only and does not replace medical advice. Please speak with a qualified healthcare professional for personal guidance.
Call to Action: Every woman’s journey is unique. If you or a loved one is going through early puberty or an early pregnancy, remember—you’re not alone. Talk to a trusted doctor, and don’t hesitate to seek support from family, friends, or community health services. Early care can protect lifelong health.