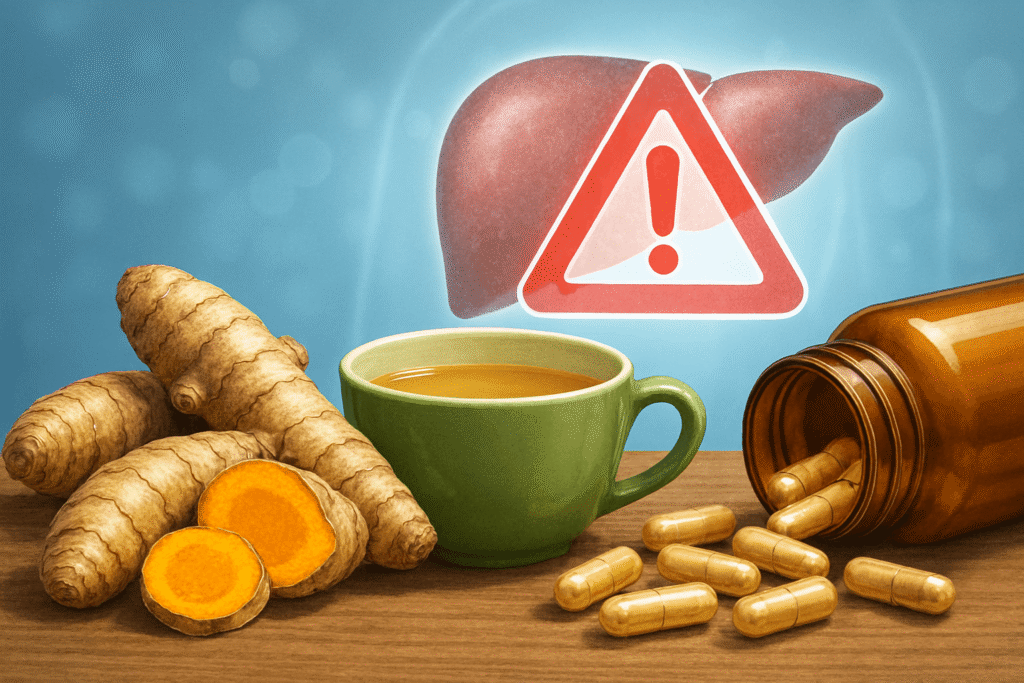
Herbal supplements liver risk from turmeric and green tea
Can herbal supplements harm your liver? Learn what evidence says about turmeric, green tea, and other herbs — risks, signs, and how to stay safe.
Turmeric to green tea: Can herbal supplements put the liver in danger?
Herbal supplements are everywhere. They promise better health. They sound natural. Yet natural does not always mean safe. In recent years, doctors have linked some popular herbal supplements to liver damage. In this article, we look at the evidence. We focus on turmeric and green tea. We also cover what increases risk. Finally, we offer practical steps to reduce harm.
Why look at herbal supplements liver risk?
Millions of people use herbal supplements. They are sold as pills, powders, and extracts. People take them for mood, energy, weight loss, inflammation, and more. Sales have soared. Yet regulation is looser than for prescription drugs. That matters. It means products vary in dose, purity, and added ingredients. Thus, risk can also vary. Several studies and clinical reports show that herbs can cause liver injury. This is called HILI — herbal-induced liver injury. PMC, NCBI
(Authoritative overviews on HILI explain the prevalence, diagnostic challenges, and examples of implicated botanicals; see LiverTox and the DILIN reviews.)
Links: LiverTox overview on herbal and dietary supplements — https://www.ncbi.nlm.nih.gov/books/NBK548441/; HDS review (DILIN) — https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5502701/. NCBI, PMC
Which herbs are most linked to liver problems?
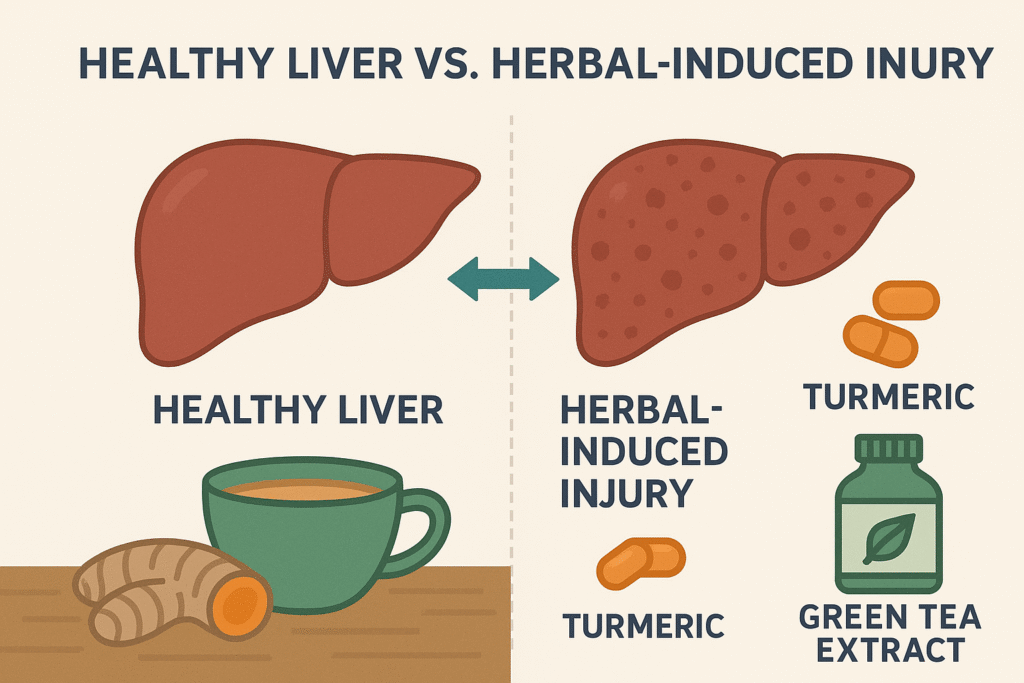
Some herbs appear more often in reports. These include green tea extract, kava, black cohosh, and, more recently, turmeric/curcumin supplements. Weight-loss and bodybuilding supplements also show up in many cases. Importantly, most cases are rare. Still, the patterns matter. Green tea extract has decades of case reports. Turmeric-linked reports have been increasing and have drawn attention in recent years. NCBI, JAMA Network
Useful reading: LiverTox green tea entry — https://www.ncbi.nlm.nih.gov/books/NBK547925/; JAMA Network report on exposures — https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2821951. NCBI, JAMA Network
Focus: turmeric — friend or risk?

Turmeric (Curcuma longa) is a common spice. Its active compound is curcumin. Small trials suggest benefits for inflammation and even some liver conditions. That said, concentrated turmeric supplements differ from culinary turmeric. They deliver high doses. Some formulations add piperine (black pepper extract) to boost absorption. That can increase how much curcumin reaches the body.
In the past decade, clinicians have reported cases of liver injury after people took turmeric or curcumin supplements. Symptoms typically appear weeks to months after starting the supplement. In some cases, liver enzymes rose substantially. A few cases were serious. Investigators suspect that high doses, enhanced-bioavailability formulas, and possibly individual genetic susceptibility may play roles. NCBI, PMC
Read more: LiverTox turmeric entry — https://www.ncbi.nlm.nih.gov/books/NBK548561/; DILIN reports and case series on turmeric. NCBI, PMC
How turmeric might cause liver injury (herbal supplements liver risk)
Scientists are still figuring this out. Possible mechanisms include:
- Direct toxicity at high concentrations.
- Idiosyncratic immune reactions in susceptible people.
- Interactions with added ingredients (for example, piperine).
- Contamination or mislabeling of the product.
Also, some turmeric supplements contain other herbs or chemicals. That makes it hard to know which compound actually caused the injury. More chemical analysis of products is needed. bhm.scholasticahq.com, MDPI
Focus: green tea extracts — a long-recognized suspect
Green tea, as a brewed beverage, is safe for most people. But green tea extracts (GTE) used in supplements have been linked repeatedly to liver injury. Case reports have documented acute, sometimes severe, hepatitis after GTE or powdered green tea supplements. The European Food Safety Authority (EFSA) and other panels have raised flags about GTE at certain doses. Genetic factors (for example, HLA variants) and states like fasting or dieting may increase risk. NCBI, Xia & He Publishing
For more: LiverTox green tea page — https://www.ncbi.nlm.nih.gov/books/NBK547925/; EFSA statements on green tea catechins. NCBI, Committee on Toxicity
Why green tea extracts can hurt the liver
GTE contains concentrated catechins like EGCG. At high doses, EGCG can stress liver cells. Some people show an immune-like liver injury pattern. Others have direct toxic changes. Notably, many GTE hepatotoxicity cases involved people using weight-loss products or taking high-strength extracts for extended periods. Also, low food intake (fasting) seems to amplify toxicity in some reports. PMC, Xia & He Publishing
How common is this problem?
HILI remains relatively rare compared with how many people use supplements. However, under-reporting is likely. Many people do not tell clinicians about supplement use. Also, when a supplement has multiple ingredients, pinpointing the cause is tough. Large surveillance networks like DILIN and national toxicology registries help identify trends. Recent population surveys show notable exposure rates to potentially hepatotoxic botanicals such as turmeric and green tea. JAMA Network, PMC
See JAMA Network exposure estimate — https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2821951. , JAMA Network
Who is at greater risk?
Certain factors raise the odds:
- Existing liver disease.
- Heavy alcohol use.
- Taking multiple drugs or supplements that affect the liver.
- High doses or long-term use of the supplement.
- Products that include bioavailability enhancers (e.g., piperine).
- Fasting or crash dieting (noted with some green tea cases).
- Individual genetic susceptibility (research suggests some HLA types). Xia & He Publishing, MDPI
What symptoms should you watch for?
Stop the supplement and see a doctor if you notice:
- Yellowing of skin or eyes (jaundice).
- Dark urine.
- Pale stools.
- Severe fatigue.
- Abdominal pain, especially upper right side.
- Persistent nausea or vomiting.
If liver tests (ALT, AST, bilirubin) are elevated, clinicians may suspect HILI and investigate supplements as potential causes. PMC
Practical steps to lower your herbal supplements’ liver risk
- Talk to your doctor before starting any supplement. This is crucial if you have liver disease or take medications.
- Prefer culinary amounts over concentrated supplements when possible. Turmeric in food rarely causes problems.
- Avoid very high doses unless supervised by a clinician.
- Be cautious with formulations claiming “bioavailability boosters” like piperine. They may raise exposure.
- Check product quality: choose reputable brands with third-party testing when possible.
- Report any side effects. If you have liver symptoms, stop the product and seek care.
- Tell your healthcare provider about all supplements and OTC products you use. This helps them spot interactions or causes of liver injury. NCBI+1
For guidance and case data, see DILIN and LiverTox resources. PMC, NCBI
Should you stop turmeric or green tea altogether?
Not necessarily. Many people use these products without harm. The key is balance and awareness. If you have risk factors, ask a clinician. If you use concentrated extracts, monitor for symptoms. Remember: evidence suggests that most cases are idiosyncratic and rare. But “rare” does not mean “impossible” for you. Weigh benefits against risks. Medical News Today, NCBI
Bottom line: herbal supplements liver risk — be smart, not scared
Herbal supplements can offer benefits. They can also carry risks. Green tea extract and turmeric supplements are two well-documented examples where concentrated forms have been linked to liver injury in some people. The risk is generally low, but not zero. You can reduce your risk by talking to a healthcare provider, choosing reputable products, avoiding unnecessary high doses, and watching for symptoms. If in doubt, use food forms instead of concentrated pills. Stay informed. Safety matters more than marketing claims.
Selected reading and resources (hyperlinks)
- LiverTox: Turmeric (curcumin) — https://www.ncbi.nlm.nih.gov/books/NBK548561/. NCBI
- LiverTox: Green Tea — https://www.ncbi.nlm.nih.gov/books/NBK547925/. NCBI
- DILIN review: Liver Injury from Herbal and Dietary Supplements — https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5502701/. PMC
- JAMA Network Open: Estimated Exposure to Potentially Hepatotoxic Botanicals — https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2821951. JAMA Network
- EFSA & green tea catechins — relevant EFSA documents and evaluations. (See EFSA webpages on catechins and hepatotoxicity.) Committee on Toxicity
Medical Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified health provider with any questions you may have regarding a medical condition, supplement use, or possible side effects. Never disregard professional medical advice or delay in seeking it because of something you have read here.
Call to Action
Your liver works hard to keep you healthy — return the favor. Talk to your healthcare provider before starting any herbal supplement, especially if you have liver disease, take medications, or plan to use high-dose extracts. If you’ve experienced side effects from a supplement, share your experience with others and report it to your doctor. Stay informed, choose wisely, and protect your liver health today.




I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?