
Couple starting intermittent fasting for fatty liver before a healthy meal
Is intermittent fasting the key to reversing fatty liver? See what trials and guidelines say, plus safe, practical tips you can use.
Intermittent Fasting for Fatty Liver: Cure or Fad?
We hear big claims. Intermittent fasting promises weight loss, better blood sugar, and even a healthier liver. But can it reverse liver disease? Or is it just another diet trend? Let’s unpack the science, step by step, and keep it simple.
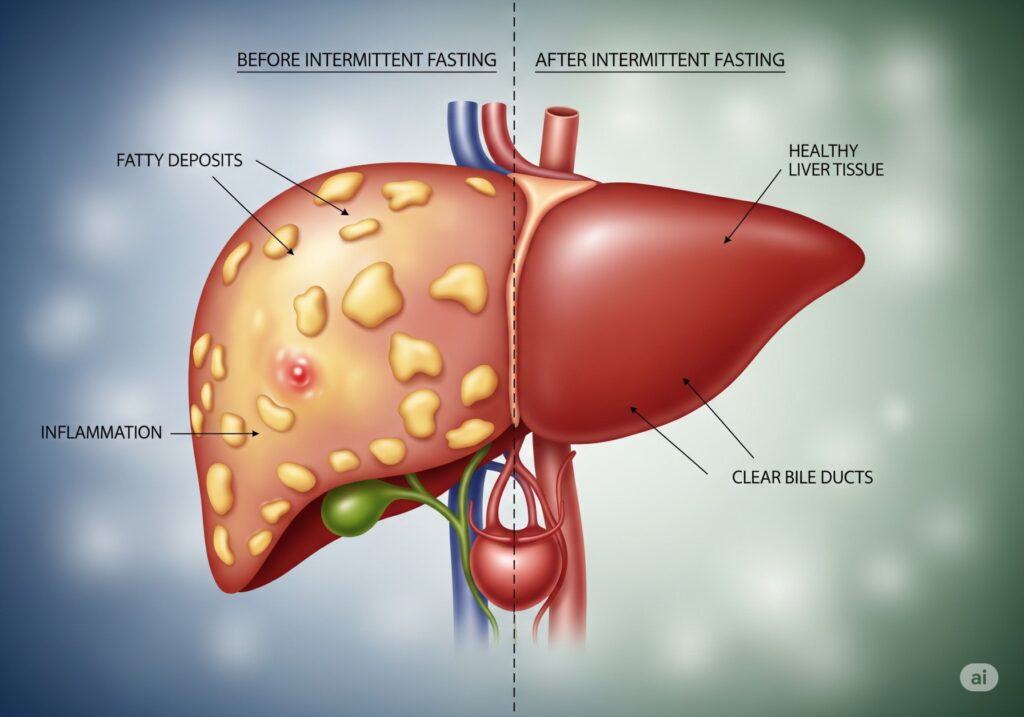
First, a quick primer on liver disease
Most headlines today point to MASLD (formerly NAFLD). That stands for metabolic dysfunction–associated steatotic liver disease. In short, fat builds up in the liver. Sometimes it inflames the organ and causes scarring (now called MASH, formerly NASH). Left unchecked, it can progress to fibrosis, cirrhosis, and complications. Lifestyle change remains the foundation of care. In fact, losing 7–10% of body weight is linked to improved liver fat, inflammation, and even fibrosis in some cases. PubMed Central, Gastrojournal+1
What exactly is intermittent fasting?
Intermittent fasting (IF) is an eating pattern, not a specific food list. Common forms include:
- Time-restricted eating (TRE): Eat within a daily 8–10-hour window.
- Alternate-day fasting (ADF): Alternate fasting days (or very low-calorie days) with normal eating days.
- 5:2 plan: Two very low-calorie days per week; regular intake the other five.
These styles aim to lower average calorie intake and improve metabolic health—often without strict calorie counting. A 2024 BMJ review found that IF approaches produce weight loss similar to continuous calorie restriction overall. BMJ
The core question: intermittent fasting for fatty liver—does it work?
Short answer: promising, but not magic. Here’s the evidence, in plain language.
Meta-analyses and reviews
A 2023 systematic review in Hepatology Communications concluded that IF can improve liver markers and reduce weight in adults with NAFLD/MASLD. However, the authors called for more and longer trials. In other words, encouraging, yet still early. (study). Lippincott Journals
A 2023–2024 narrative and umbrella review line also suggests that TRE can reduce liver fat and stiffness. But researchers remain cautious about issuing blanket recommendations until larger randomized studies confirm durability and safety across different groups. (open-access review). Frontiers
Randomized controlled trials (the gold standard)
- Time-restricted eating (TRE): Multiple RCTs report reductions in liver fat, weight, and waist size with daily eating windows (often 8–10 hours). One trial reported improved steatosis even without explicit calorie counting. (PubMed abstract). PubMed
- Alternate-day fasting (ADF): A randomized trial showed that three months of ADF (with or without aerobic exercise) significantly reduced intrahepatic triglyceride (IHTG) content in people with NAFLD. Interestingly, adding exercise did not always beat fasting alone for liver fat reduction. (trial, open access; PubMed). PubMed Central, PubMed
- 5:2 vs daily calorie restriction: A 2024 RCT in NAFLD compared a 5:2 style plan with standard daily calorie cuts. Both improved weight and metabolic markers. The 5:2 approach worked, but it did not clearly outperform traditional calorie restriction. (trial, open access). Frontiers
- Most recent TRE evidence: Newer 2025 RCT results in Journal of Hepatology (early online) report that 16 weeks of TRE improved key hepatic endpoints versus standard care and performed comparably to calorie restriction. This suggests TRE may be as effective as classic dieting for liver fat control, while some people find it easier to follow. (abstract). ScienceDirect
Takeaway: IF helps many patients lose weight and reduce liver fat. But it does not consistently beat a well-done, calorie-restricted diet. The best plan is the one you can sustain. BMJ
But can IF reverse liver disease?
Here’s the nuance. In early disease (fatty liver without significant scarring), reducing liver fat and inflammation is very possible with weight loss, achieved via IF or other methods. Resolution of steatohepatitis and even regression of fibrosis have been linked to ≥10% total body weight loss, regardless of diet type. IF is one road to that weight loss, not the only one. (AASLD/AGA guidance & studies, AASLD explainer). AASLD+1
So yes, some patients can see reversal of disease features, but the driver is sustained weight loss and healthier metabolism—not fasting per se. IF is a tool, not a cure.
What do liver societies say today?
Guidelines still emphasize overall calorie deficit + physical activity as first-line therapy. They consider TRE/IF a reasonable option to achieve that deficit for those who prefer it, but not a universally superior method. The 2023 AASLD practice guidance and recent summaries underscore weight loss targets and exercise as the cornerstones. (AASLD Practice Guidance; slides summary). AASLD, Emory School of Medicine
Mechanisms: why intermittent fasting for fatty liver can help
Short fasting windows may:
- Improve insulin sensitivity and lower hepatic fat production.
- Increase fat burning and reduce liver fat stores.
- Support modest weight loss without constant calorie counting.
But again, similar benefits appear when people consistently cut calories and move more. The diet pattern you’ll actually stick to wins. BMJ
Where intermittent fasting shines—and where it doesn’t
Potential advantages
- Simpler rules: eat within a window; no micromanaging every bite.
- Natural calorie reduction for many.
- Works about as well as classic diets for weight and glycemia. (BMJ 2024). BMJ
Potential limitations
- Not clearly superior to daily calorie restriction.
- Evening social eating and shift work can make strict windows hard.
- Some people overeat during feeding windows and stall progress.
Safety first: who should not rely on fasting?
This part matters. People with advanced liver disease (cirrhosis) face high risks of malnutrition and muscle loss. For them, guidelines often discourage prolonged fasting and even recommend late-evening snacks to protect muscle and metabolism. In short, minimize long fasting gaps if you have cirrhosis. (AASLD clinical pearls; Hepatology guidance statements). AASLD, Lippincott Journals
Also, be cautious if you:
- Use insulin or sulfonylureas (risk of low blood sugar).
- Are you pregnant or breastfeeding?
- Have a history of disordered eating.
- Have chronic kidney disease or other complex conditions.
Rapid weight loss can also raise gallstone risk and may not be appropriate for everyone. Slow, steady loss is safer. Talk to your clinician first. (overview on gallstone/NAFLD overlap). CGH Journal
What about Ramadan or religious fasts?
Short-term religious fasts create natural TRE cycles. For most healthy people, brief periods are safe. But if you have cirrhosis, diabetes on medications, or high malnutrition risk, ask your doctor for an adjusted plan. Frequent small meals and avoiding long night fasts are often advised in cirrhosis. (ESPEN & clinical nutrition guidance; 2024 clinical nutrition review). PubMed Central, ScienceDirect
Practical, safe steps to try intermittent fasting for fatty liver

If your clinician clears you, start small. Keep it sustainable.
- Pick a gentle TRE window: Try 12:12 first, then 10:14, and only then 8:16 if it still feels good. No need to rush.
- Prioritize quality: During your eating window, go for a Mediterranean-style plate—vegetables, legumes, whole grains, nuts, olive oil, fish, and lean proteins. Keep added sugars low. This pattern is strongly tied to better liver and heart health. (Guidance slide deck). Emory School of Medicine
- Aim for steady weight loss: About 0.25–0.5 kg/week is a safe pace. Remember, the big liver wins show up around 7–10% total weight loss. PubMed Central
- Move daily: Mix aerobic and resistance training. Both reduce liver fat and protect muscle. (lifestyle guidance). Gastrojournal
- Mind the evenings: Late-night snacking can creep in. Keep a consistent window and a simple routine.
- Hydrate and sleep: Both influence appetite and insulin sensitivity.
- Monitor labs: Track ALT/AST, lipids, glucose, weight, and waist. Share results with your clinician.
Where does the science stand today?
- IF is effective for many people with MASLD/NAFLD, mainly by enabling weight loss and metabolic improvements. Lippincott Journals, PubMed, PubMed Central
- IF is not clearly superior to standard calorie restriction for liver outcomes across the board. Choose the method you can stick with. BMJ
- Reversal of disease features can happen when weight loss is large and sustained (≈10%). That’s the real lever, whichever diet gets you there. Gastrojournal
- People with cirrhosis should avoid long fasts and focus on adequate protein and energy with short meal gaps. Lippincott Journals
So…secret weapon or fad?
Neither. Intermittent fasting is a useful tool—often simple, flexible, and effective. But it’s not a cure on its own. The real “secret” is sustainable habits that drive steady weight loss and better metabolic health. IF can help you do that. If it fits your life, it’s a keeper. If it doesn’t, a classic Mediterranean-style, calorie-reduced plan works just as well.
FAQs about intermittent fasting for fatty liver
Does TRE work if I don’t count calories?
Often, yes. TRE naturally trims intake for many people, and trials show improved liver fat and weight with daily 8–10-hour eating windows. But some still need gentle calorie awareness. (trial abstract). PubMed
Is ADF better than TRE?
Not necessarily. ADF can reduce liver fat, but adherence varies. Choose the pattern you can maintain. (trial). PubMed Central
Will IF reverse fibrosis?
It can, indirectly, through substantial weight loss. Studies link ≥10% weight loss with fibrosis improvement, regardless of diet. (AASLD/AGA data). Gastrojournal
What do guidelines recommend right now?
Create a calorie deficit, increase physical activity, and consider patterns like TRE if they help you stick to the plan. (AASLD guidance). AASLD
The bottom line
Intermittent fasting can reduce liver fat, lower weight, and improve metabolic health. That’s great news. However, it’s not a miracle, and it’s not mandatory. If you like the structure, use it. If not, pick a different route to the same destination: steady weight loss, better food quality, and daily movement.
Before you start, especially if you take glucose-lowering medications or have advanced liver disease, talk to your clinician. Safety first.
Key sources to explore further:
- AASLD Practice Guidance on MASLD/MASH (2023): clinical priorities and weight-loss targets. (AASLD). AASLD
- 2023 meta-analysis on IF in NAFLD: promising but more RCTs needed. (Hepatology Communications). Lippincott Journals
- RCTs on TRE and ADF in NAFLD. (TRE abstract; ADF trial). PubMed PubMed Central
- 2024 BMJ review: IF ≈ calorie restriction for weight loss. (BMJ). BMJ
- Nutrition guidance in cirrhosis: Avoid prolonged fasting. (Hepatology guidance statements). Lippincott Journals
Medical Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified health provider before starting any diet, fasting plan, exercise program, or making changes to your treatment. Never disregard professional medical advice or delay seeking it because of something you have read here.
Call to Action
Your liver health is too important to leave to guesswork. If you’re considering intermittent fasting or making lifestyle changes, speak with your healthcare provider to create a safe, personalized plan. Share this article with friends or family who may benefit, and follow us for more evidence-based tips on protecting and improving your health.




1 thought on “New Research Reveals How Intermittent Fasting for Fatty Liver Works”