kidney diagram showing calcium deposits caused by vitamin D toxicity
Learn how Vitamin D toxicity causes hypercalcemia, harms the kidneys and the heart, and what to do to stay safe. Clear signs, causes, and treatments.
Vitamin D toxicity: How excess Vitamin D can harm your kidneys and heart
Vitamin D is essential. It helps bones, immunity, and more. Yet too much can be dangerous. In particular, the kidneys and heart are at risk. This article explains how. It also shows causes, signs, tests, and treatment. Above all, it gives clear steps to stay safe.
What is Vitamin D toxicity?
Vitamin D toxicity — also called hypervitaminosis D — happens when vitamin D intake raises blood calcium too high. In short, extra vitamin D increases calcium absorption from the gut. Then, blood calcium rises. This condition is called hypercalcemia. Many symptoms follow. The main cause is too much supplement intake rather than sun exposure or food. Authoritative reviews and fact sheets explain this mechanism and common causes. Office of Dietary Supplements, PMC
(See NIH fact sheet: Vitamin D — Health Professional Fact Sheet and StatPearls overview: Vitamin D Toxicity – StatPearls.)
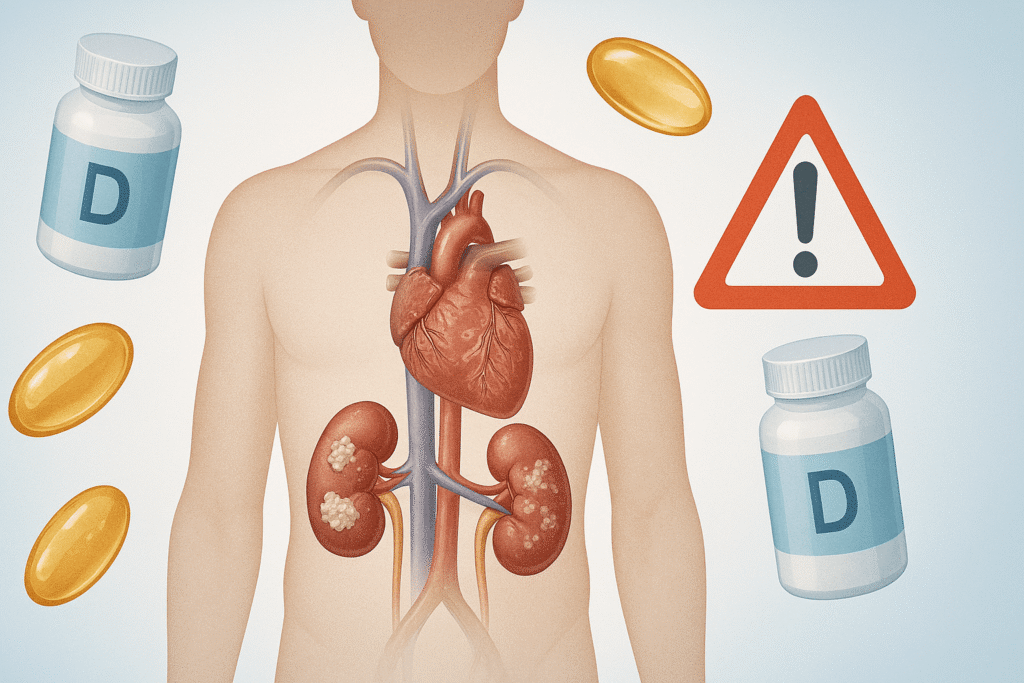
Why the kidneys suffer from Vitamin D toxicity (Vitamin D toxicity and kidney damage)
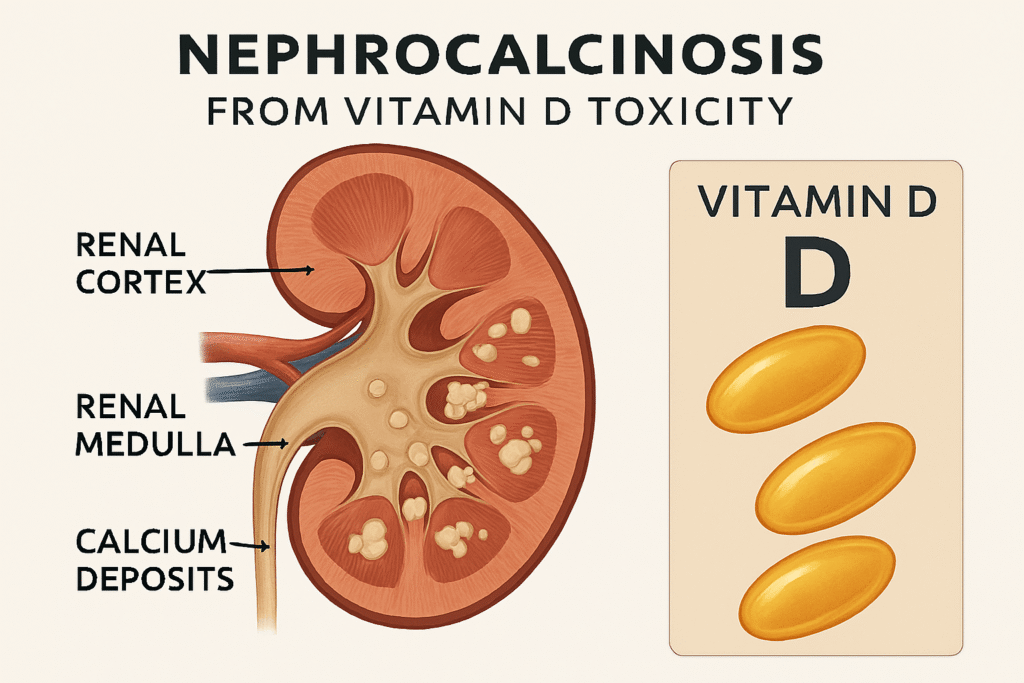
The kidneys filter blood. They also help remove excess calcium. When calcium is high, kidneys face two problems. First, they must clear extra calcium. Second, calcium crystals can form. Over time, these crystals can injure kidney tissue. As a result, people may develop kidney stones, nephrocalcinosis (calcium deposits in kidney tissue), and even acute or chronic kidney failure. Clinical case reports show that very high vitamin D doses have caused acute renal failure and severe hypercalcemia. PMC+1
In practice, kidneys also get dehydrated. This happens because high calcium makes people pass more urine. That leads to low blood volume. Then kidney blood flow drops. Therefore, kidney function worsens. Simple hydration helps, but severe cases sometimes need hospital care.
How hypercalcemia harms the kidneys (H3: How Vitamin D toxicity damages kidneys)
- High urine calcium (hypercalciuria) increases stone risk.
- Calcium deposits (nephrocalcinosis) scar kidney tissue.
- Low blood volume from polyuria reduces kidney filtration.
- In severe cases, toxins build up and dialysis may be required.
Medical reviews and case reports document these steps and explain the typical findings. If you take very high doses of supplements, kidney injury can follow over weeks to months. PMC+1
How hypercalcemia harms the kidneys ( How Vitamin D toxicity damages kidneys)
- High urine calcium (hypercalciuria) increases stone risk.
- Calcium deposits (nephrocalcinosis) scar kidney tissue.
- Low blood volume from polyuria reduces kidney filtration.
- In severe cases, toxins build up and dialysis may be required.
Medical reviews and case reports document these steps and explain the typical findings. If you take very high doses of supplements, kidney injury can follow over weeks to months. PMC+1
How the heart is affected by Vitamin D toxicity (Vitamin D toxicity and heart problems)
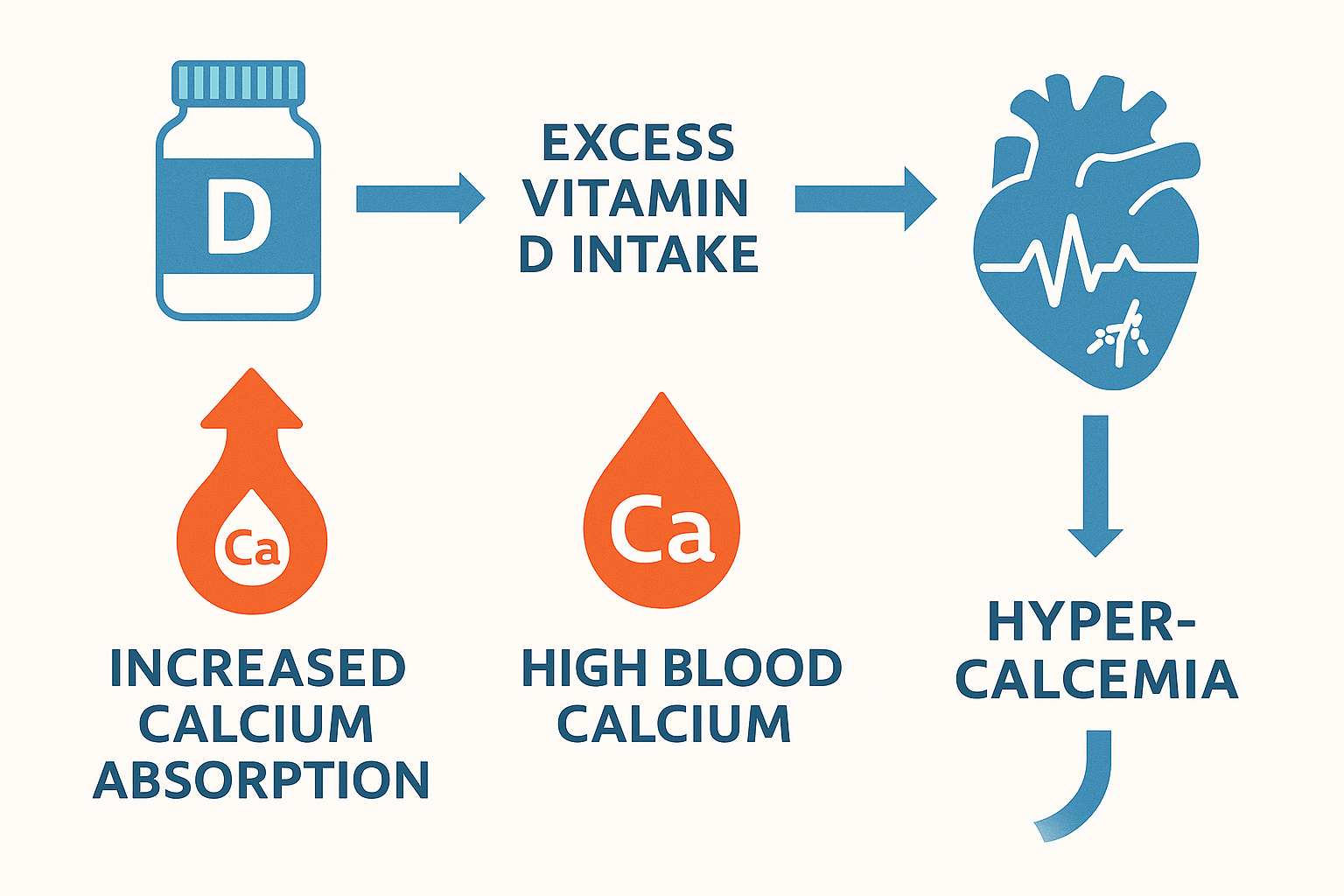
High blood calcium affects the heart’s electrical system. In turn, this can cause arrhythmias — abnormal heart rhythms. Severe hypercalcemia also raises blood pressure and may lead to changes in heart muscle size. Over time, high calcium can encourage calcium to deposit in blood vessel walls. That promotes vascular stiffness and may increase cardiovascular risk. Reports of fatal outcomes tied to extreme vitamin D overdose highlight these dangers. Mayo Clinic. Business Insider
Importantly, the heart effects are usually secondary to hypercalcemia. So controlling calcium levels is key to protecting the heart.
Specific cardiac risks (Heart complications from Vitamin D toxicity)
- Irregular heartbeats (arrhythmias).
- Shortened QT interval on ECG.
- Hypertension and left ventricular hypertrophy.
- Vascular calcification and stiffness.
Clinical literature links severe hypercalcemia with these cardiac findings. Thus, extreme overdose—though rare—can be life-threatening. Mayo Clinic Proceedings, PMC
Who is at risk?
Most people are safe with usual doses. Yet certain groups face higher risk:
- People are taking very high-dose vitamin D supplements.
- Patients are given multiple supplements or compounded prescriptions.
- Those taking vitamin D plus calcium supplements.
- People with granulomatous diseases (like sarcoidosis) or certain lymphomas that raise active vitamin D locally.
- Patients with kidney disease who cannot clear excess calcium well.
The NIH and clinical reviews stress that most toxicity cases come from supplement misuse or manufacturing errors. Always check labels and dosages. Office of Dietary Supplements, PMC
How much vitamin D is too much?
There is no single toxic cutoff that applies to everyone. However, general guidance helps:
- Daily recommended amounts are small (e.g., 600–800 IU for many adults).
- Toxicity usually appears after prolonged intake of very high doses. Typical reports involve thousands to tens of thousands of IU daily, or massive single doses.
- Extremely high 25-OH vitamin D serum levels (often >150 ng/mL or >375 nmol/L) are seen in toxicity cases.
In short, do not assume “more is better.” Follow recommended doses unless a clinician prescribes otherwise. For people on high therapeutic doses, doctors usually monitor blood levels. Office of Dietary Supplements, PMC
Symptoms to watch for
Vitamin D toxicity symptoms reflect hypercalcemia. Common signs include:
- Nausea and vomiting.
- Loss of appetite and weight loss.
- Excessive thirst and frequent urination.
- Fatigue, weakness, and confusion.
- Muscle pain and bone pain.
- Kidney pain or reduced urine output in severe cases.
If you have several symptoms and you take high-dose supplements, see a clinician and get blood tests. Early action can prevent serious damage. Mayo Clinic, PMC
How doctors diagnose Vitamin D toxicity
Diagnosis relies on tests:
- Measure serum calcium (total and ionized).
- Check serum 25-hydroxyvitamin D (25-OH D) level.
- Measure urine calcium.
- Review medication/supplement history.
- In some cases, test for underlying conditions (parathyroid hormone, granulomatous disease workup).
If vitamin D toxicity is suspected, stop supplements immediately. Then clinicians treat the hypercalcemia and its complications. StatPearls and clinical reviews outline this approach. NCBI, PMC
Treatment and what to expect
Treatment focuses on lowering blood calcium and protecting organs:
- Stop vitamin D and calcium supplements.
- Give intravenous isotonic saline to restore volume and increase calcium excretion.
- Use diuretics like furosemide in hospital settings to increase calcium loss (under supervision).
- In severe cases, medications such as bisphosphonates, glucocorticoids, or calcitonin may be used.
- Dialysis is reserved for life-threatening cases or severe kidney failure.
Most people improve with proper treatment and monitoring. However, if organ injury (kidney or heart) is advanced, recovery can be slow or incomplete. Therefore early detection matters. NCBI, PMC
Real cases and regulatory concerns
Case reports show real harm. For example, severe toxicity and renal failure occurred when supplement doses were much higher than labeled amounts. Manufacturing errors and unregulated high-dose products have caused life-threatening hypercalcemia. These reports prompted calls for better labeling and oversight. Always buy from reputable brands and avoid high-dose products unless prescribed. PMC, Business Insider
(See case reports: Vitamin D intoxication presenting as acute renal failure and review: A review of the growing risk of vitamin D toxicity.)
Practical tips to stay safe
- Take vitamin D only at recommended doses or as your doctor prescribes.
- Avoid combining multiple supplements unless you check total vitamin D and calcium.
- If you are on high doses, ask your doctor for periodic blood tests (25-OH D, calcium, kidney function).
- Stay hydrated, especially if you feel thirsty or urinate often.
- If you take prescription vitamin D, confirm the exact dose. Mislabeling can occur with compounded or non-regulated products.
Simple steps reduce risk. Monitoring is key for those on large doses.
When to see a doctor
Seek urgent care if you have any of the following while taking vitamin D supplements:
- Severe nausea, vomiting, confusion, or fainting.
- Little or no urine for many hours.
- Rapid or irregular heartbeat.
- Severe muscle weakness or difficulty breathing.
Tell the clinician about all supplements you take. Bring bottles to show exact doses.
Bottom line
Vitamin D is vital. But excess vitamin D can cause serious harm. The harm happens mostly through hypercalcemia. In turn, hypercalcemia can damage the kidneys and disrupt heart function. Most cases arise from excessive supplement use or faulty products. Therefore, use supplements sensibly. If you need high doses for medical reasons, get regular blood tests and medical supervision.
Selected sources and further reading
- NIH Office of Dietary Supplements — Vitamin D (Health Professional Fact Sheet). Office of Dietary Supplements
https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/ - Mayo Clinic — Vitamin D toxicity: What if you get too much? Mayo Clinic
https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/vitamin-d-toxicity/faq-20058108 - StatPearls — Vitamin D Toxicity. NCBI
https://www.ncbi.nlm.nih.gov/books/NBK557876/ - Case report — Vitamin D intoxication presenting as acute renal failure (PMC). PMC
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2813130/ - Review — A review of the growing risk of vitamin D toxicity from inappropriate practice. PMC
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5980613/
Medical Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified health provider with any questions you may have regarding your health, supplements, or a medical condition. Never disregard or delay seeking professional advice because of something you have read here. If you think you may be experiencing symptoms of Vitamin D toxicity or any other medical emergency, call your doctor or emergency services immediately
Call to Action
Your health matters — don’t leave it to guesswork. If you take vitamin D supplements, talk to your healthcare provider about the right dose for your needs. Share this article with friends and family so they can also learn the risks of excess vitamin D. Stay informed, stay safe, and make your health decisions backed by expert guidance.