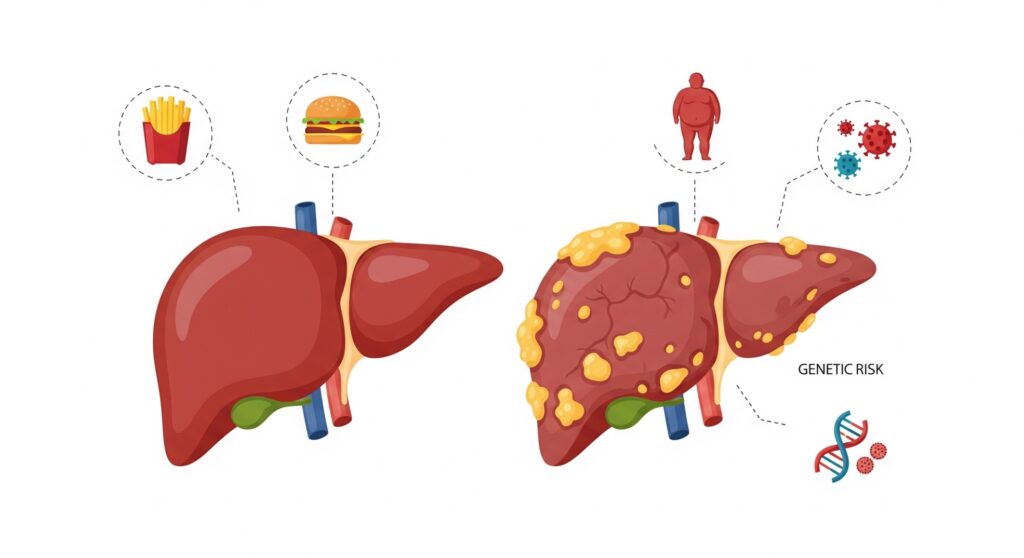
Non-drinkers' liver disease comparison between healthy and damaged liver
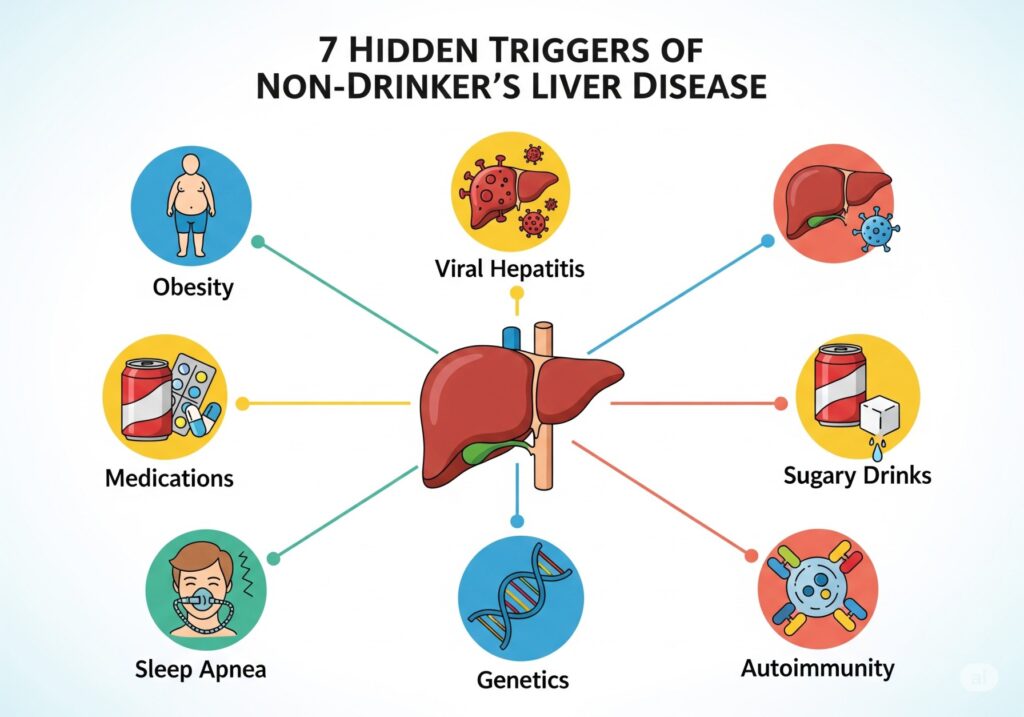
Many people who don’t drink still develop liver problems. Learn 7 hidden triggers of non-drinkers’ liver disease and how to lower your risk.
Why Even Non-Drinkers Get Liver Disease – The 7 Hidden Triggers
You don’t need to drink alcohol to hurt your liver. In fact, millions of people who rarely drink still develop liver damage. Doctors even updated the name of the most common condition to reflect that truth. Nonalcoholic fatty liver disease is now called metabolic dysfunction–associated steatotic liver disease (MASLD)—a reminder that metabolism, not alcohol, drives much of today’s liver illness. AASLD, PMC, Journal of Hepatology
Below, you’ll find seven surprising triggers behind non-drinkers’ liver disease, plus practical steps to protect yourself.
1) Metabolic dysfunction (MASLD): the modern engine of damage
Excess body fat, insulin resistance, and type 2 diabetes push fat into the liver. Over time, that fat sparks inflammation and scarring. This is MASLD. It now sits under a broader umbrella, steatotic liver disease (SLD), and often travels with high blood pressure, abnormal cholesterol, and central obesity. The good news? Weight loss, better sleep, regular activity, and balanced eating can slow or reverse early changes.
Learn more: AASLD: New MASLD nomenclature | 2024–25 clinical guidance. AASLD, Journal of Hepatology
How this feeds non-drinkers’ liver disease: metabolic stress quietly injures liver cells day after day. PMC
2) Viral hepatitis B & C: infections that fly under the radar
You can get hepatitis B or C through blood, unsterile injections, or from mother to baby. Many people feel fine for years; meanwhile, the virus inflames the liver and raises cancer risk. The CDC now recommends one-time hepatitis B screening for all adults, while the WHO urges broader HCV testing and simplified treatment. If you’ve never been screened, ask your doctor.
Start here: CDC—Hepatitis B screening | WHO—Hepatitis C fact sheet. CDC, World Health Organization
Why it matters for non-drinkers’ liver disease: you can have zero alcohol intake and still develop chronic hepatitis–related cirrhosis. Early testing saves livers. World Health Organization
3) Medications that tax the liver (and supplements that surprise you)
Plenty of everyday drugs can injure the liver in certain people. High-dose acetaminophen is a well-known culprit; others include amiodarone, methotrexate, and more. Many “natural” products are not harmless either—green tea extract, multi-ingredient bodybuilding or weight-loss supplements, and certain herbs have been linked to liver injury. Always share your full medication and supplement list with your clinician.
Authoritative resources: MedlinePlus: Drug-induced liver injury | NIH LiverTox (drug/herb database) | AASLD guidance on DILI. MedlinePlus, NCBI, Lippincott Journals
Connection to non-drinkers’ liver disease: injury can occur without alcohol, and it often looks like other liver illnesses—making disclosure and monitoring crucial. NCBI
4) “Healthy” diets that hide risky ingredients: fructose & ultra-processed foods
Too much fructose from sugary drinks and sweets promotes liver fat, insulin resistance, and inflammation. High intake of ultra-processed foods (UPFs) is also linked to higher odds of fatty liver in population studies. Shift toward minimally processed foods, fiber, lean proteins, and unsweetened beverages.
Evidence: Recent reviews on fructose and MASLD and on UPFs and NAFLD risk:
- Review of fructose & MASLD
- UPFs and NAFLD—systematic reviews/meta-analyses | 2025 update | BMJ umbrella review on UPFs & health. PMC+2PMC+2BMJ
Why it fuels non-drinkers’ liver disease: sugar-sweetened drinks and ultra-processed patterns drive metabolic dysfunction—even in people who never drink alcohol. Nature
5) Obstructive sleep apnea (OSA): night-time oxygen dips, daytime liver harm
If you snore loudly, wake unrefreshed, or feel daytime sleepiness, OSA could be at play. Intermittent low oxygen levels worsen insulin resistance and liver fat accumulation. Studies link OSA to higher odds and severity of MASLD. Getting tested and treating OSA (often with CPAP) may help metabolic and liver health.
Read more: 2025 analysis of OSA–NAFLD association | Narrative review. PMC, Frontiers
Tie to non-drinker’s liver disease: poor sleep and untreated apnea amplify metabolic stress on the liver. Frontiers
6) Autoimmune hepatitis: when your immune system attacks the liver
Sometimes, the body’s immune defenses mistakenly target liver tissue. Autoimmune hepatitis can progress silently, then present with fatigue, joint pain, or abnormal liver tests. Early diagnosis and immunosuppressive therapy can prevent scarring.
Learn more: AASLD—Autoimmune hepatitis | StatPearls overview. AASLD, NCBI
Relevance to non-drinker’s liver disease: alcohol isn’t required; immune misfires alone can inflame and scar a liver. NCBI
7) Genetics you can’t see: iron and copper overload
Two inherited conditions quietly injure the liver:
- Hereditary hemochromatosis causes iron overload. Without treatment, iron deposits can lead to cirrhosis and cancer. Simple blood tests (ferritin, transferrin saturation) and genetic testing can confirm it, and phlebotomy removes excess iron. See: CDC—Hemochromatosis. CDC, NCBI
- Wilson’s disease leads to copper buildup, often in teenagers and young adults, but it can present at any age. Chelation and zinc therapy save lives when started early. See: MedlinePlus Genetics | StatPearls. MedlinePlus, NCBI
Why this causes non-drinker’s liver disease: inherited metal overload injures the liver with no alcohol involved—and family screening can catch cases early. CDC
Spotting trouble early (and what to do next)
Because many of these triggers are silent, screening matters:
- Ask for a liver panel if you have metabolic risks, OSA, or a family history of liver disease.
- Get HBsAg (hepatitis B) and HCV tests at least once in adulthood, per public-health guidance. Vaccinate against hepatitis B if not immune. CDC HBV screening | WHO HCV testing & treatment. CDC, World Health Organization
- Review all medications and supplements with your clinician; check new products on NIH LiverTox. NCBI
- If you snore or feel excessively sleepy, discuss sleep apnea testing. PMC
- With iron or copper disorders in the family, ask about genetic testing and targeted labs. CDC
Everyday protection plan for non-drinkers’ liver disease

Small, consistent steps add up:
- Move more, sit less. Aim for brisk walking most days; add resistance training twice weekly.
- Choose minimally processed foods. Favor vegetables, fruit, legumes, whole grains, nuts, seeds, eggs, fish, and plain yogurt. Limit sugary drinks and ultra-processed snacks. BMJ, PMC
- Sleep 7–9 hours and treat snoring or OSA. Frontiers
- Keep vaccines current. Hepatitis A/B protection is a powerful liver shield (ask your clinician for your schedule).
- Know your numbers. Track waist size, blood pressure, lipids, glucose, and liver enzymes.
The bottom line
Alcohol isn’t the only path to liver damage. Metabolic dysfunction, silent viral infections, medications and supplements, sleep apnea, autoimmunity, and inherited iron or copper overload can all drive non-drinkers’ liver disease. The earlier you look, the more you can do—often with simple lifestyle steps, screening, and targeted treatment. If any trigger above feels familiar, book a check-up and ask specifically about your liver risk.
Note: This article is for educational purposes and isn’t a substitute for medical advice. Always consult a qualified healthcare professional for diagnosis and treatment.




6 thoughts on “7 Causes of Non-Drinkers’ Liver Disease You Must Know”